Diabetes
Menin acts like a brake
on beta cell regeneration
We can set beta cells free
Read More
CONTENTS
SIDEBAR-CONTENT-1
Pipeline
The following table summarizes our product candidate pipeline. We own full worldwide development and commercialization rights to all of our programs.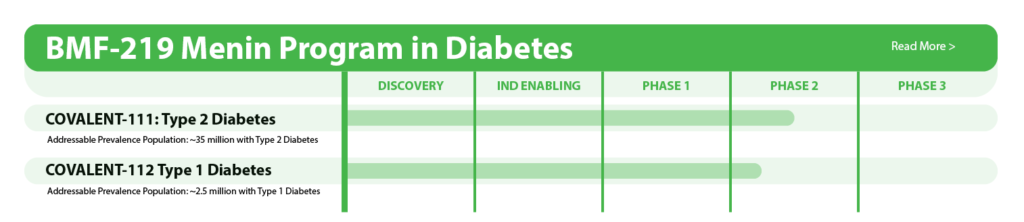
All our assets are in house designed, developed, and wholly owned by Biomea Fusion Inc.
About Diabetes
Diabetes is a chronic health condition that affects the how the body metabolizes nutrients. It results in too much glucose (sugar) in the bloodstream. Over time, this can cause serious health problems by damaging vital tissues and organs. Most people with diabetes have a shorter life expectancy than people without this disease. The Centers for Disease Control (CDC) estimates about 2 in 5 adults in the USA are expected to develop diabetes during their lifetime. More than 37 million people of all ages (about 11% of the US population) have diabetes today. 96 million adults (more than 1 in 3) have prediabetes, glucose levels that are higher than normal but not high enough to be classified as diabetes. Diabetes is also one of the largest economic burdens on the US health care system with $1 out of every $4 in US health care costs being spent on caring for people with diabetes.
Beta cells are found in the pancreas and are responsible for the synthesis and secretion of insulin. Insulin is a hormone that helps the body use glucose for energy and helps control blood glucose levels. In patients with diabetes, beta-cell mass and function are diminished, leading to insufficient insulin secretion and elevated glucose levels (hyperglycemia).
There are two major types of diabetes: type 1 diabetes (T1D) and type 2 diabetes (T2D). T1D is caused by an autoimmune reaction (the body “attacks itself” by mistake). This reaction destroys insulin producing beta cells in the pancreas, stopping the body’s ability to produce and secrete insulin. Approximately 5-10% of the people who have diabetes have T1D. With T2D, the body doesn’t use insulin well and can’t keep blood sugar at normal levels. About 90-95% of people with diabetes have T2D. Loss of functional beta-cell mass is a core component of the natural history in both T1D and T2D.
Despite significant advances in pharmacotherapy and diabetes-related devices over the past 2 decades, it is estimated that approximately 50% of persons with diabetes in the US do not have adequate glucose control, as defined by a glycated hemoglobin (HbA1C) of 7% or less. One important reason is that current agents for the management of T2D and T1D do not address the root cause of diabetes – a progressive decline in beta-cell mass and function.
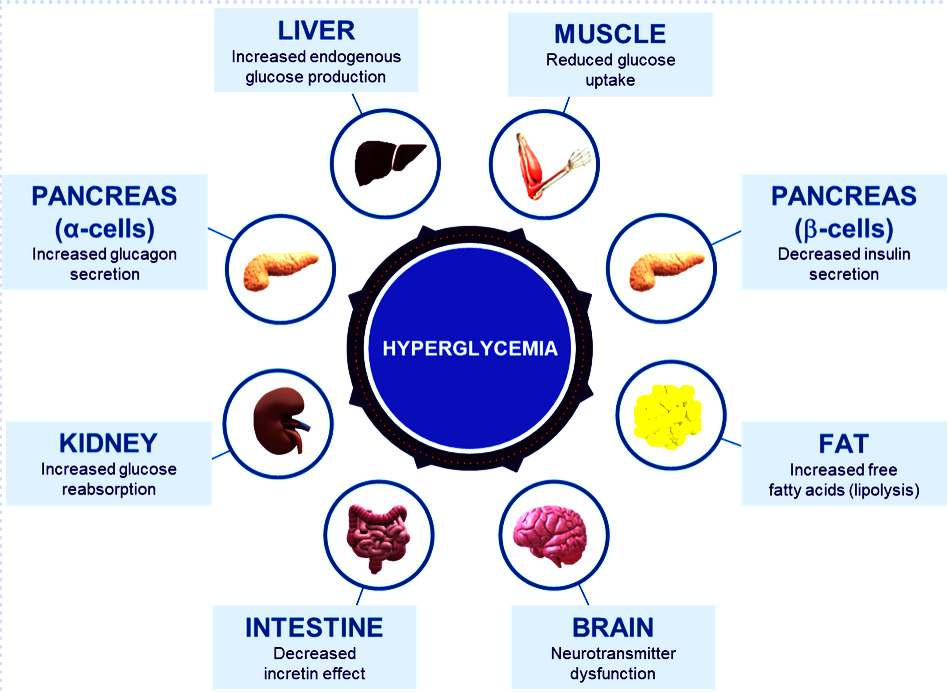
Fig. Different abnormalities that contribute to the hyperglycemia that occurs in patients with T2D (adapted from DeFronzo et al. Diabetes 2009)
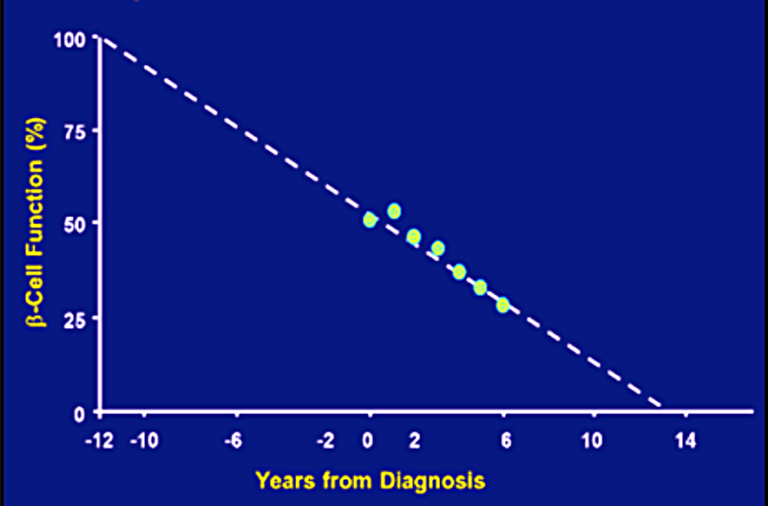 Fig. Progressive decline in beta-cell function (Lebovitz et al. Diabetes Review 1999)
Fig. Progressive decline in beta-cell function (Lebovitz et al. Diabetes Review 1999)
SIDEBAR-CONTENT-2
Menin in Diabetes
Menin is a transcriptional scaffold protein that controls the expression and activity of proteins that regulate beta-cell proliferation. Menin is thought to control beta-cell proliferation and mass by acting as a brake on beta-cell turnover / beta-cell growth, supporting the notion that inhibition of menin could lead to the regeneration of normal, healthy beta cells, which could be a disease-modifying approach to treat diabetes.
BMF-219 – Mechanism of Action
BMF-219, is an orally bioavailable, potent and selective covalent inhibitor of menin, built from our FUSION™ System. Loss of functional beta cell mass is a core component of the natural history in both types of diabetes — type 1 diabetes (mediated by autoimmune dysfunction) and type 2 diabetes (mediated by metabolic dysfunction). Beta cells are found in the pancreas and are responsible for the synthesis and secretion of insulin. Insulin is a hormone that helps the body use glucose for energy and helps control blood glucose levels. In patients with diabetes, beta cell mass and function have been observed to be diminished, leading to insufficient insulin secretion and hyperglycemia. Menin is thought to act as a brake on beta-cell turnover and growth, supporting the notion that inhibition of menin could lead to the regeneration of normal, healthy beta cells.
BMF-219’s proposed mechanism of action in diabetes is to enable the proliferation, preservation, and reactivation of a patient’s own healthy, functional, insulin-producing beta cells. As the potentially first disease-modifying therapy for type 1 and type 2 diabetes, BMF-219 could be an important addition and complement to the treatment landscape, if approved.
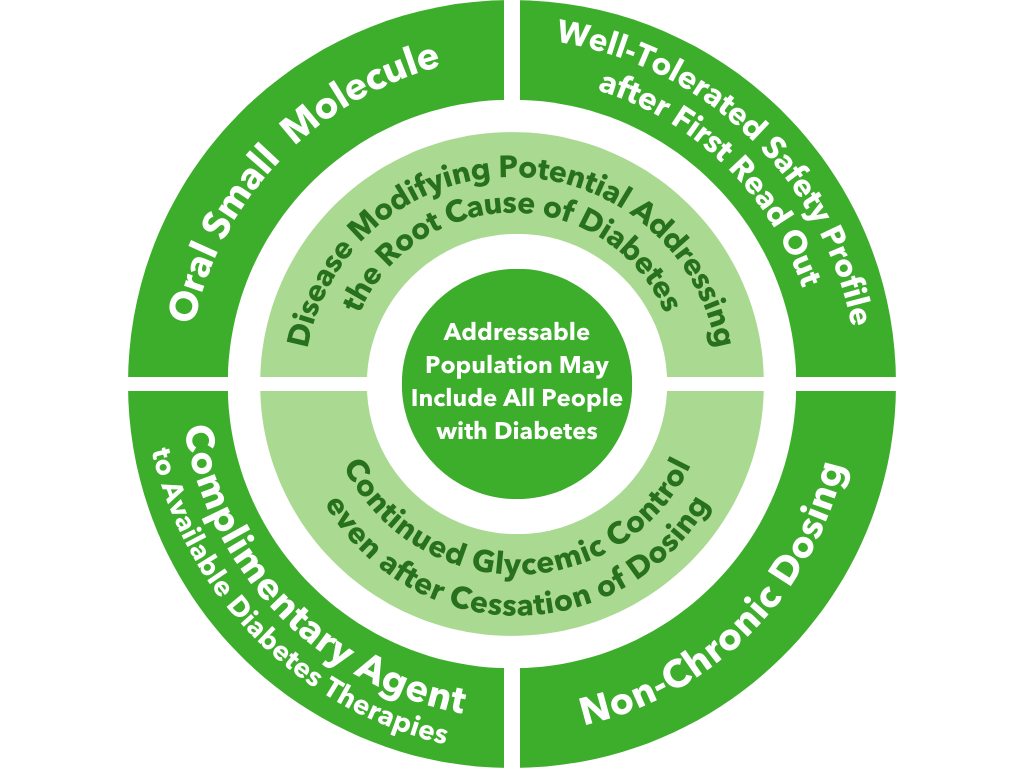
Fig. BMF-219’s unique value proposition
Preclinical Development
Biomea conducted two diabetes animal experiments to measure the potential impact of BMF-219 for the treatment of type 2 diabetes: the Zucker Diabetic Fatty (ZFD) Rat, a widely studied model of obesity and insulin resistance in rats, and the Streptozotocin (STZ) induced rat, a widely studied model by which diabetes is induced using an antibiotic (STZ) that destroys beta cells. In both models, BMF-219 was able to normalize glucose levels in the majority of animals after just 2 weeks of treatment. Notably, the majority of the effect was maintained despite complete washout of BMF-219. (Butler et al, EASD 2022; Somanath et al. EASD 2022).
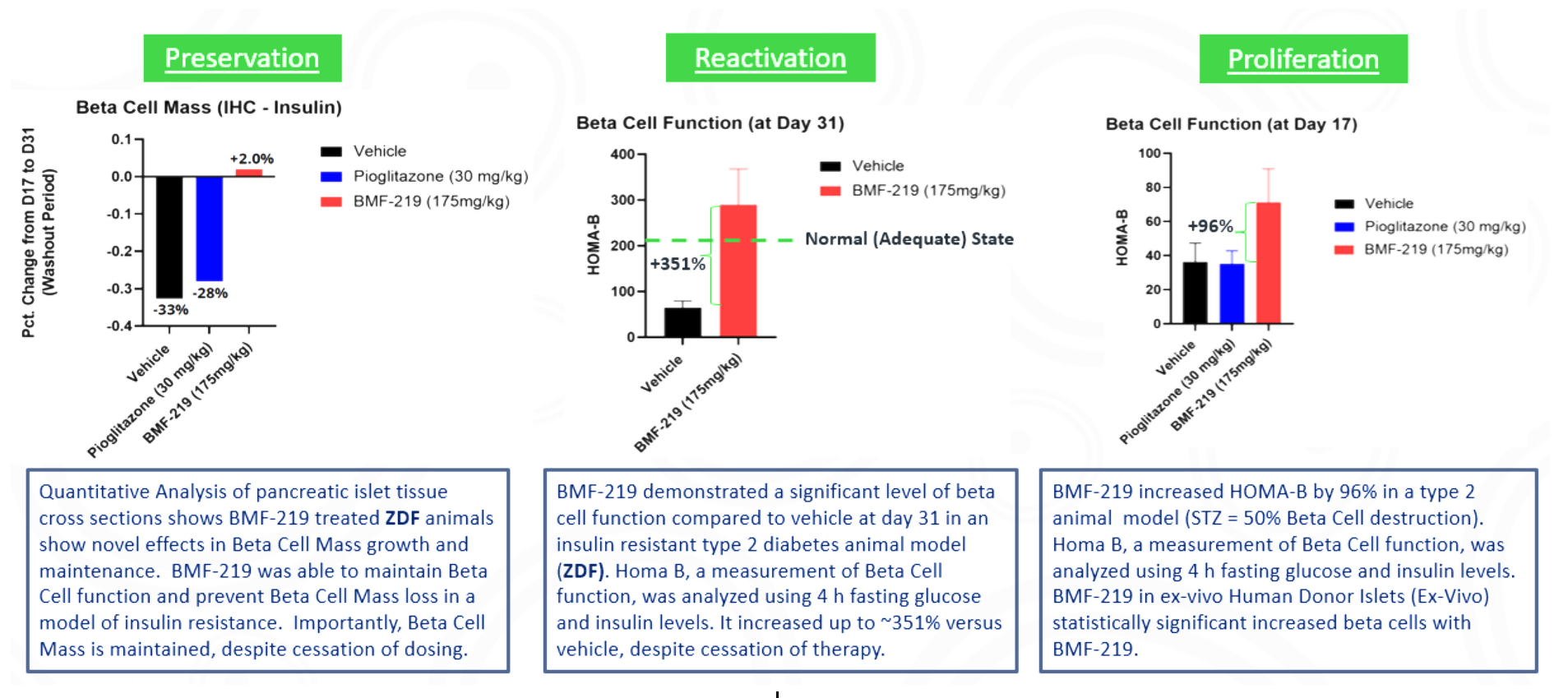
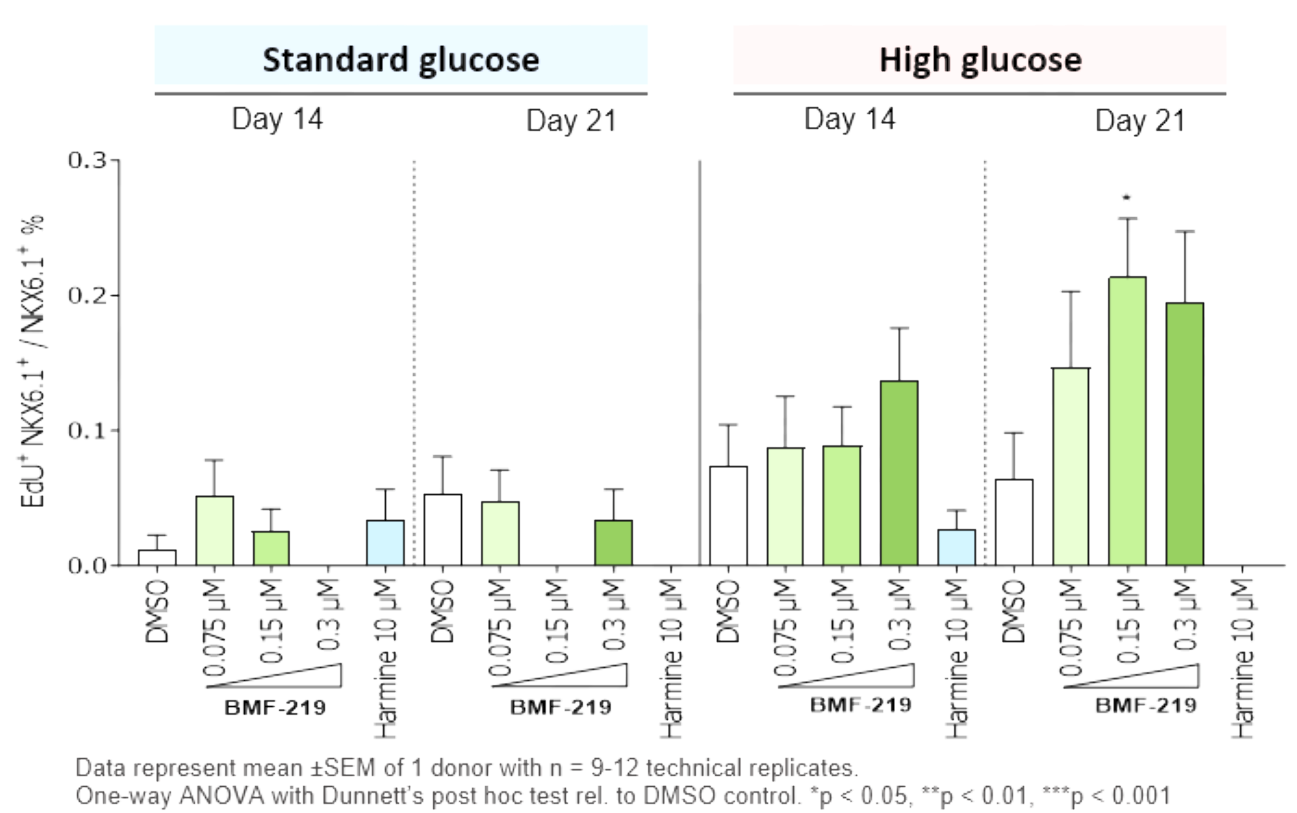
In addition in December 2023, preclinical ex vivo human islet data was presented. Dependent on dose concentration and also dependent on dose duration, BMF-219 was observed to increase beta-cell mass and function, as well as promote controlled proliferation and enhance insulin content in beta cells. Proliferation was observed only under elevated glucose conditions, which mimics diabetic levels, and with continuous drug exposure. BMF-219 was observed to upregulate the expression of key cell-cycle proteins, PbK and CCNA2 (Cyclin A2) in a glucose-dependent fashion. When not sequestered to menin, PbK expression was known to be upregulated by JunD, which is a glucose-sensitive menin binding partner. (Kulkarni et al. WCIRDC 2023)
Clinical Development
Biomea reported initial clinical data from the first two cohorts of the Phase 2 portion of COVALENT-111 (NCT05731544) in March of 2023. As reported, 89% of patients enrolled in Cohort 3 (n=10 patients at 100 mg without food) achieved a reduction in HbA1c, 78% achieved ≥ 0.5% reduction in HbA1c, and 56% achieved ≥ 1% reduction in HbA1c (median and mean reduction over the cohort: -1.0% and -0.81%, respectively). BMF-219 was well tolerated and demonstrated a favorable safety profile with no dose discontinuations.
Additional clinical data were presented in June of 2023 from the first two cohorts of patients with type 2 diabetes enrolled in the Phase 2 portion of COVALENT-111. This new data highlighted specific patients treated with BMF-219 for 4 weeks who maintained or experienced a further decrease in HbA1c levels 8 weeks after treatment was completed, up to a 2.4% reduction from baseline. (Rodriguez et al. ADA 2023)
Fig. Clinical data presented at 2023 ADA. The top 50% of responders after 4 weeks of treatment in Cohorts 2 and 3 (100 mg BMF-219 fed and fasted, respectively) demonstrated durable and ongoing reduction in HbA1c while off treatment up to Week 12; a continued reduction in HbA1c was observed in Cohort 2 (additional 114%) and in Cohort 3 (additional 62%) (Rodriguez et al. ADA 2023)
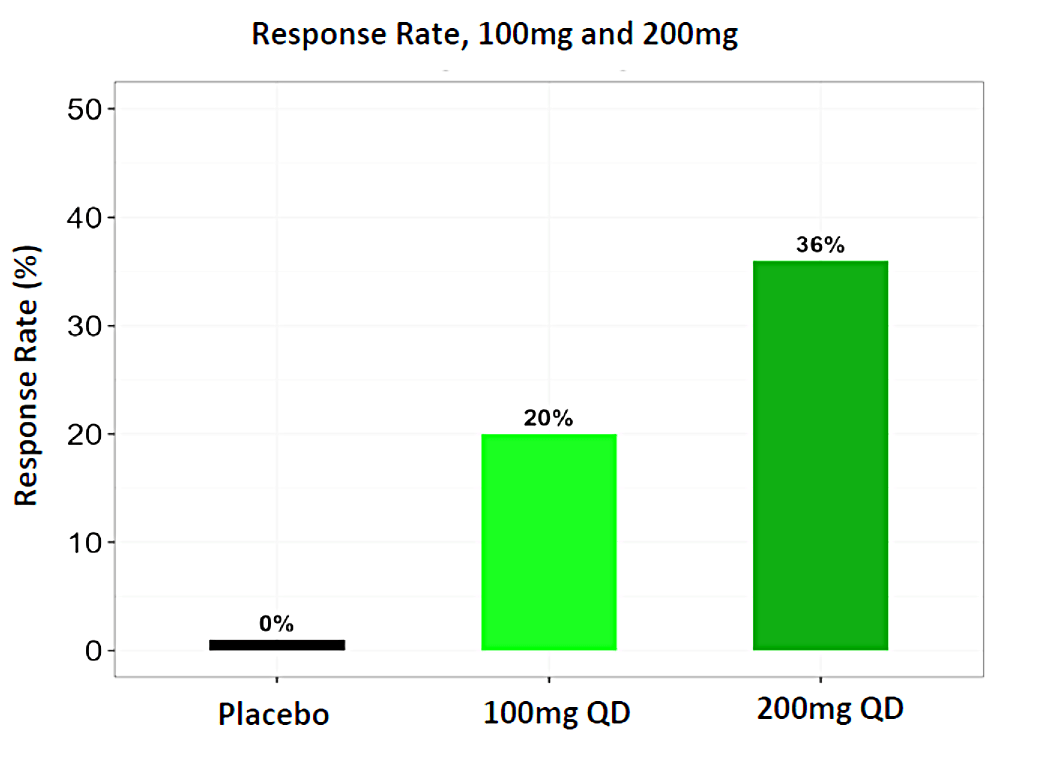
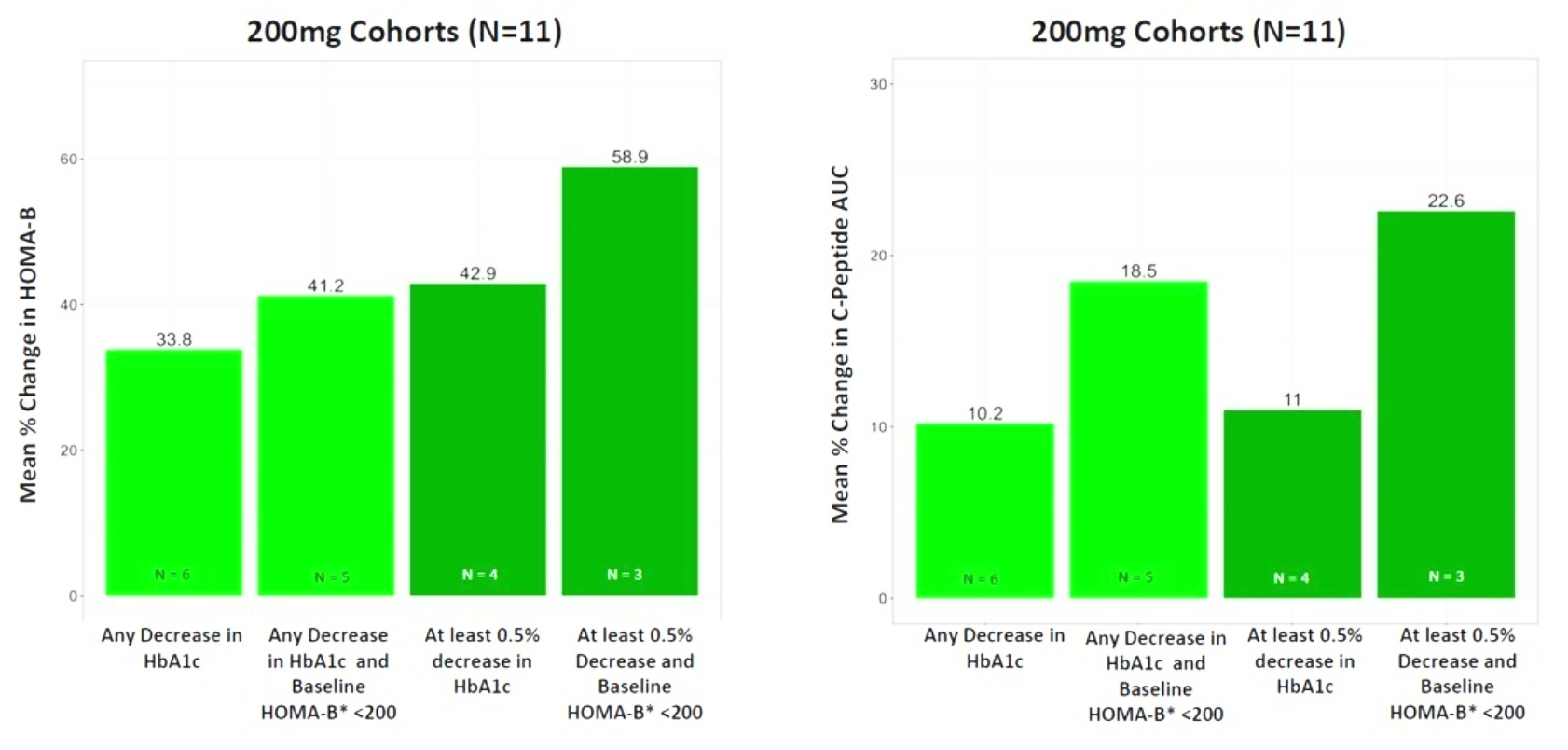
In December 2023, Biomea presented long-term follow-up data showing improved glycemic control after 22 weeks off treatment in an ongoing Phase 2 study (COVALENT-111) of BMF-219 in type 2 diabetes. At Week 26, 22 weeks after the last dose of BMF-219, participants in the 100 mg QD (without food) cohort saw an improved placebo-adjusted mean reduction in HbA1c of 0.8% (compared to a 0.7% placebo-adjusted mean reduction in HbA1c at Week 4). Observed HbA1C reduction was supported by an increase from baseline in placebo adjusted mean HOMA-B (+270%) and in mean stimulated C-peptide AUC (+22%) at Week 26 in responders (defined as HbA1c reduction ≥0.5% at Week 26) with baseline below the HOMA-B upper limit of normal (<200). BMF-219 was generally well tolerated; no dose reductions, dose discontinuations, or severe or serious adverse events, and no symptomatic or asymptomatic hypoglycemia was observed. In addition, Biomea reported that the 200 mg cohorts near doubled the percentage of patients (~36%) with durable HbA1c reduction of 1% or more compared to the 100 mg cohorts which reported earlier as 20%. (Frias et al. WCIRDC 2023)
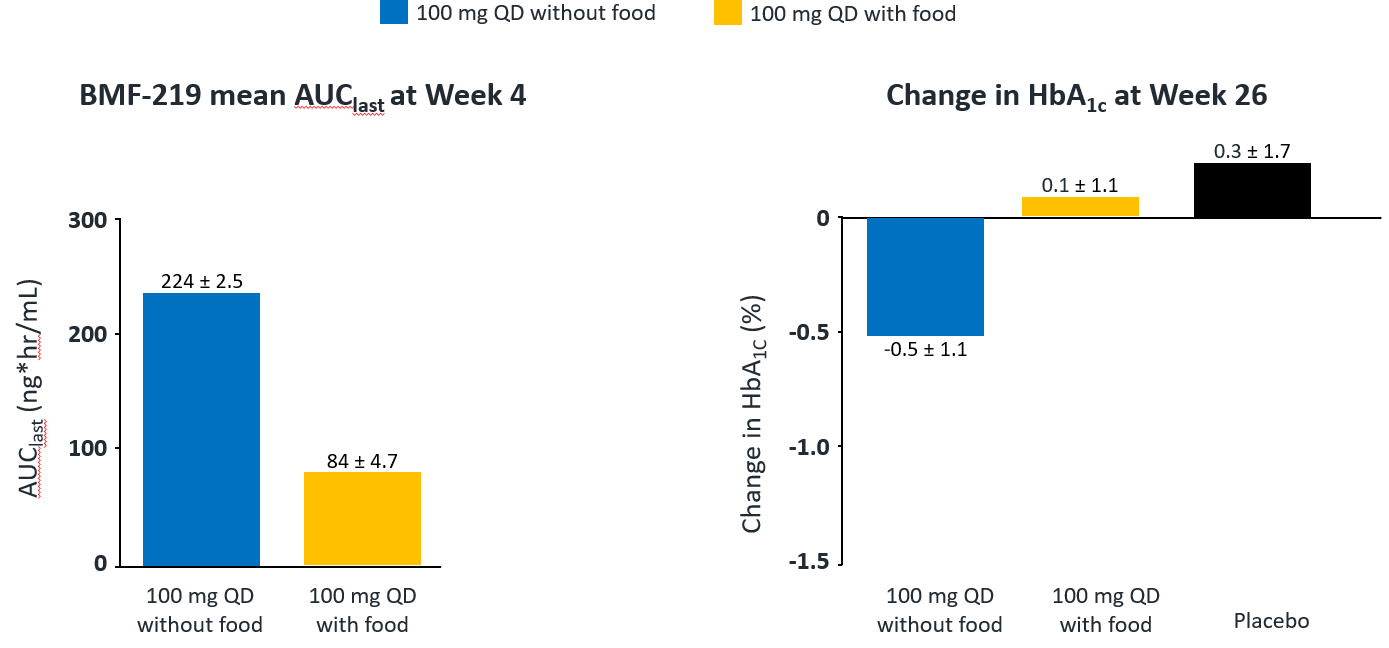
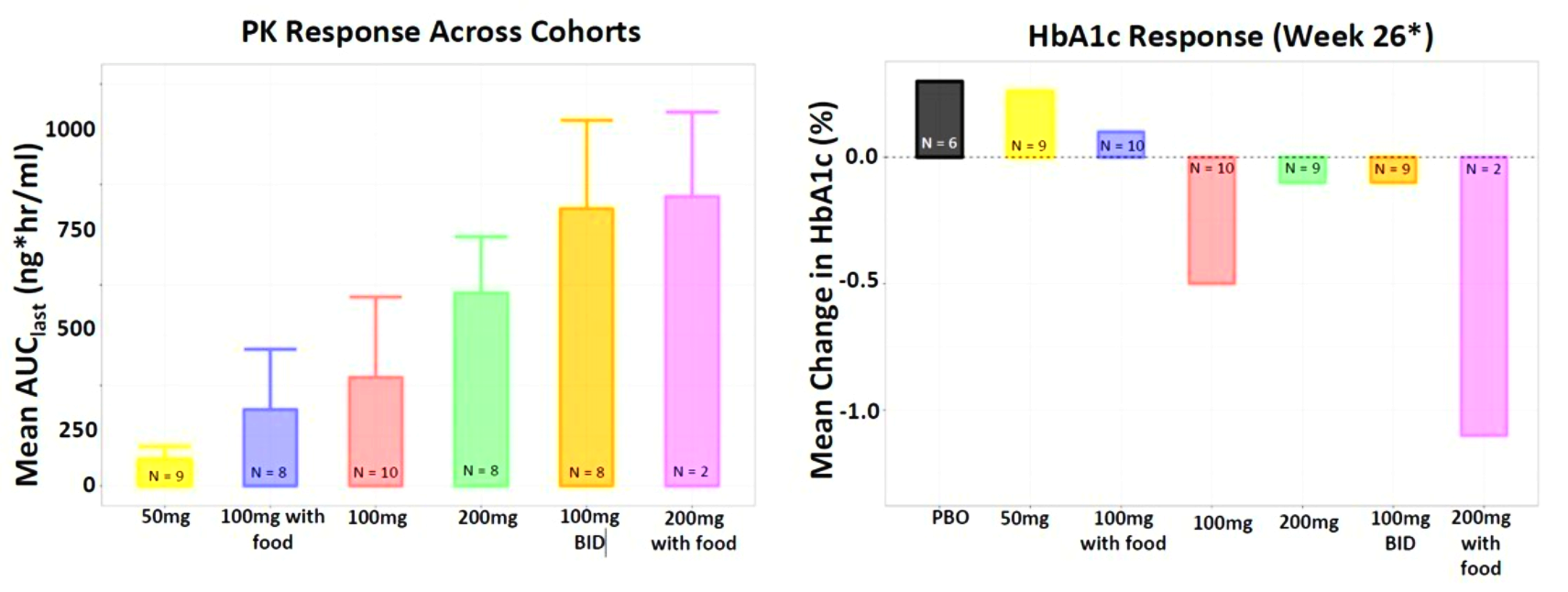
Fig. Clinical data presented at 2023 WCIRDC. Pharmacokinetics and HbA1c Response
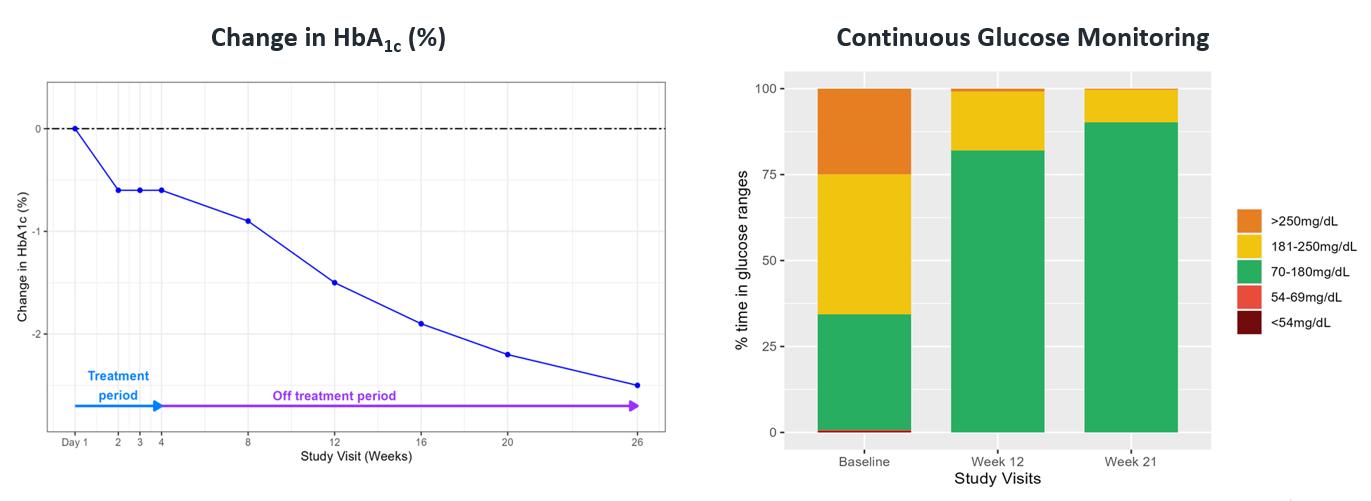
Fig. A case study of a 29-year-old man with 4-year history of T2D
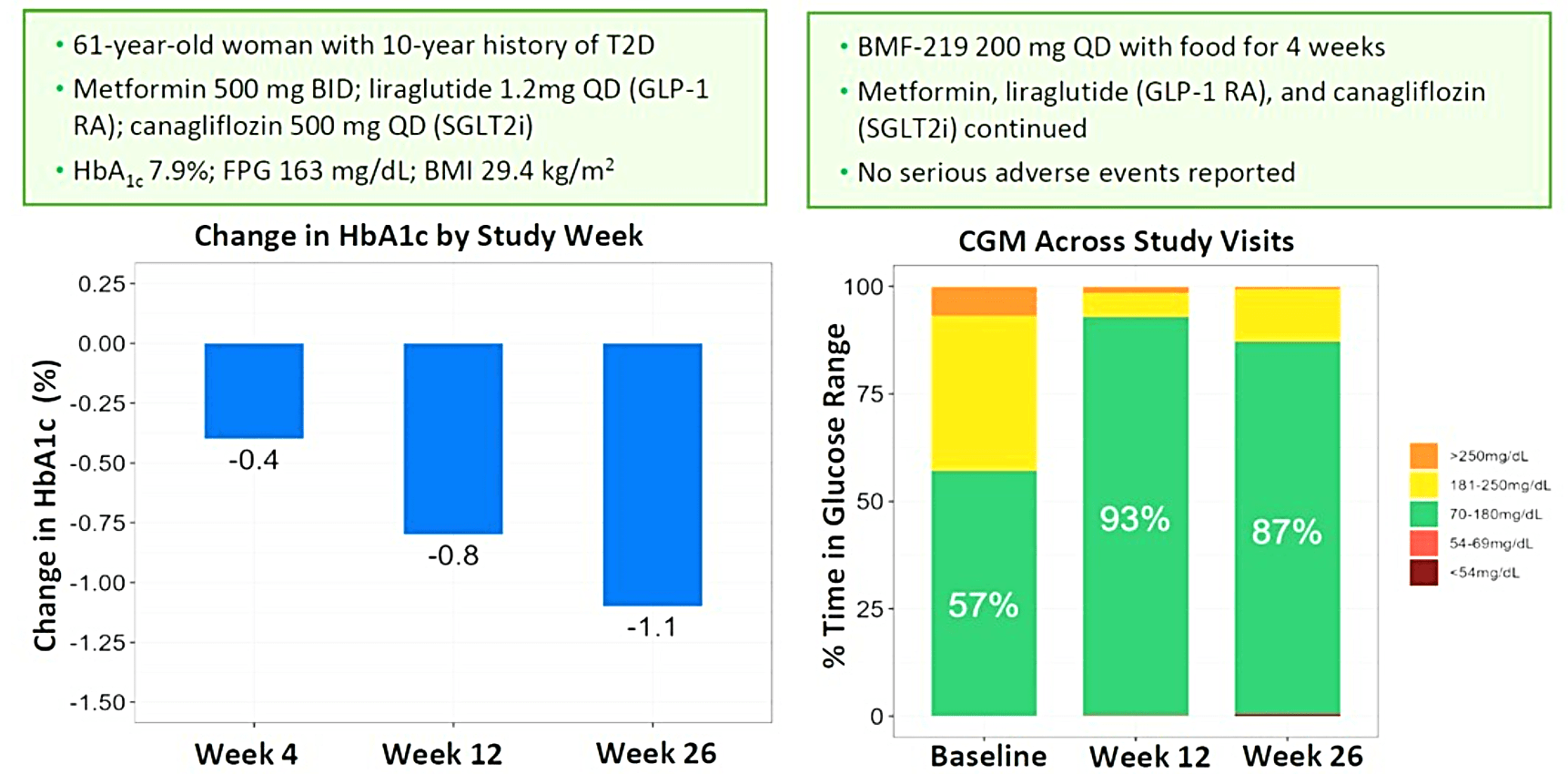
Biomea presented additional clinical data sets from the dose escalation phase of COVALENT-111 in March of 2024, highlighting BMF-219’s novel mechanism of action in patients with type 2 diabetes. Patients in COVALENT-111 are displaying improved glycemic control while off therapy, supporting improved pancreatic function following BMF-219 treatment. Patients who demonstrated the greatest HbA1c reduction at Week 26 (22 weeks off treatment) had the greatest improvement in beta cell function as measured by HOMA-B and C-peptide. In patients failing current standard of care medications, at Week 26, following a 28-day dose cycle of BMF-219, a general dose response was observed with placebo-adjusted mean percent changes of HbA1c of -0.04% (50mg QD*), -0.2% (100mg QD with food), -0.8% (100mg), -0.4% (200mg QD), -0.4% (100mg BID), and -1.4% (200mg with food) (*50mg data out to Week 20, latest data cut). Across 100mg QD, 200mg QD, and 100mg BID cohorts (N=40), 38% of patients had ≥0.5% HbA1c reduction (with a mean HbA1c reduction of 1.2%), and 23% of patients had ≥1.0% HbA1c reduction (with a mean HbA1c reduction of 1.5%) at Week 26. Patients with >7 years duration of diabetes and failing dual- or triple-agent therapy (including GLP1 RA and/or SGLT2i) (n=2) also demonstrated improved glycemic control (HbA1c -0.4%, -1.1%, and -1.1% at Weeks 4, 12, and 26, respectively) with BMF-219 dosed at 200mg with food. Increase in HOMA-B and C-peptide generally correlated with glycemic control, consistent with BMF-219’s core mechanism of action: beta-cell proliferation and improved beta-cell function. BMF-219 was generally well tolerated with no serious adverse events and no adverse event-related study discontinuations, and no symptomatic or clinically significant hypoglycemia. 100mg and 200mg dose levels have been selected for the first 3 Arms of the Expansion Phase, which will dose patients up to 12 weeks (compared to 4 weeks in the Escalation Phase) and extended follow-up to Week 52. (Rodriguez et al. ATTD 2024, Abitbol et al. ATTD 2024, Denham et al. ATTD 2024)